Bruce Willis has a progressive brain condition you may not have heard of
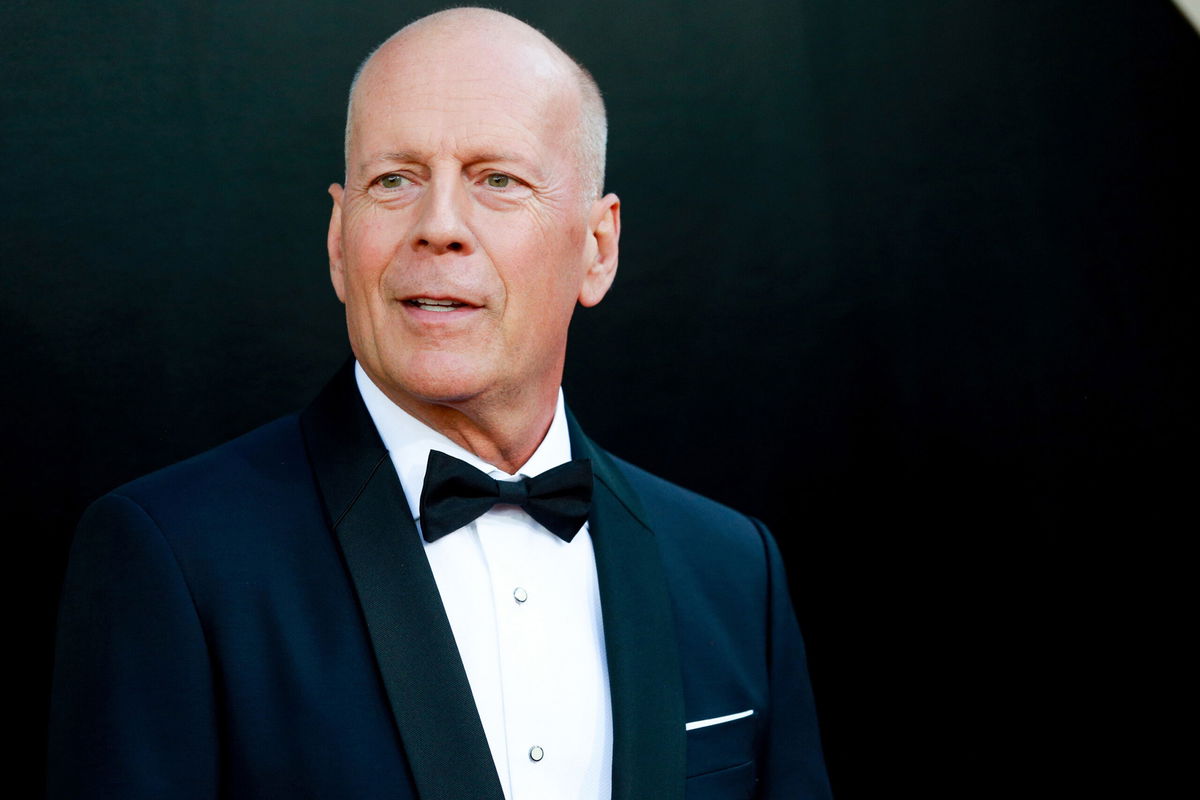
After retiring from acting in March 2022 due to a speaking disorder called aphasia
By Sandee LaMotte and Kristen Rogers, CNN
After retiring from acting in March 2022 due to a speaking disorder called aphasia, Bruce Willis, 67, has since been diagnosed with frontotemporal dementia, his family announced Thursday.
“Since we announced Bruce’s diagnosis of aphasia in spring 2022, Bruce’s condition has progressed,” the Willis family noted in a statement. “Unfortunately, challenges with communication are just one symptom of the disease Bruce faces. While this is painful, it is a relief to finally have a clear diagnosis.”
Frontotemporal dementia, or FTD, is a group of disorders caused by a buildup of tau and other brain cell destroying proteins in the brain’s frontal lobes (behind your forehead) or temporal lobes (behind your ears). The condition typically strikes between the ages of 45 and 64, according to Alzheimer’s Research UK.
“The most common dementia for people under 60, FTD can cause challenges in communication, as well as changes to one’s behavior, personality, or movement,” according to a statement from the Association for Frontotemporal Degeneration.
People with FTD typically live six to eight years with the condition, according to the US National Institute on Aging. Between 10% and 30% of FTD cases are inherited. Other than genetics, there are no other known risk factors, although researchers are investigating what role the thyroid and insulin may play in the onset of the disease.
What are the types of FTD?
Because his symptoms began with difficulty speaking, Bruce Willis would be classified as having a type of FTD called primary progressive aphasia, said Dr. Henry Paulson, a professor of neurology and director of the Michigan Alzheimer’s Disease Center at the University of Michigan.
“Aphasia really means problems with language, and that can vary from having trouble finding your words to understanding what people say. It can occur because of a tumor on the brain, a stroke or from a progressive neurodegenerative condition,” Paulson said.
“Because his diagnosis is frontotemporal dementia, Mr. Willis clearly has a progressive, neurodegenerative disease as opposed to a stroke or a tumor or some other lesion on the brain,” he added.
There are two other types of FTD. Behavior variant frontotemporal dementia, or bvFTD, is characterized by changes in executive functions, thinking and planning.
Another type affects motor neurons, and can show up via an inability to swallow, rigid muscles, and difficulty in using hands or arms to “perform a movement despite normal strength, such as difficulty closing buttons or operating small appliances,” according to the National Institute on Aging.
What are the symptoms of FTD?
In the beginning, it can be difficult to know exactly which type of FTD a person has — or even whether it is FTD — because symptoms and the order in which they appear can vary from one person to another and depend on which parts of the frontal or temporal lobes are affected.
In behavioral FTD, people rarely have issues with memory. Instead, they struggle to plan and sequence their thinking and have trouble setting priorities, according to the National Institute on Aging. They may parrot the same activity or word again and again, become disinterested in life, and act impulsively — saying inappropriate words or doing things others might perceive as embarrassing.
In primary progressive aphasia, or PPA, the person might have trouble speaking or understanding words or might slur their speech. Over time, they may fail to recognize familiar faces and objects. Some may become mute.
“PPA may start with difficulty simply finding words, so people begin to use simpler words or more generic words for things they can’t quite recall,” Paulson said.
“Now that also comes with the territory of aging, but when the language is more effortful on a daily basis, or the comprehension is going downhill, that’s a sign that someone should see a doctor for an evaluation,” he said.
Motor neuron FTD disorders may not affect memory, cognition, language or behavior, especially at first. Initial signs may include the inability to control movements, or issues with balance and walking. A hallmark sign of one of those disorders, progressive supranuclear palsy, is difficulty with looking down or other eye movements.
How is FTD diagnosed?
To diagnose FTD disorders, a neurologist will conduct a careful clinical examination, paired with psychological testing designed to evaluate cognitive skills, Paulson said.
“A brain MRI can tell us if certain parts of the brain are shrinking or showing signs of atrophy. We will do some blood tests to make sure we’re not missing some treatable causes of cognitive impairment like thyroid disease or vitamin B12 deficiency as well,” he said.
“And oftentimes, we also will do brain metabolism imaging,” Paulson said. “It’s Positron Emission Tomography or PET imaging, and that can tell us which parts of the frontal lobes or the temporal lobes are involved.”
How is FTD treated?
Unlike Alzheimer’s disease, there are no current therapies to slow down the progression of FTD. Medical professionals can attempt to improve a patient’s quality of life by prescribing medications to reduce agitation, irritability or depression.
A speech-language pathologist can help determine the best strategies and tools for an FTD patient struggling with language skills. Physical or occupational therapy, guided by a doctor specializing in these disorders, may help with movement symptoms.
“It is really important for people who have a progressive dementing syndrome like FTD to continue to eat well, exercise regularly, and stay connected with people. Those activities are not medications, they’re not curing the disease, but they can help your brain work as well as possible,” Paulson said.
As the disease progresses, patients can continue to have active, satisfying lives, adapting to their symptoms in ways that are inspiring, he added.
“I’ve seen patients who completely lose their speech and yet they go out and take their camera and take beautiful photographs of the lives they’re living. They can’t tell me in words, but they can tell me in pictures,” Paulson said.
“I tell all my patients, ‘Don’t let this disease own you. You own it,'” he added. “Sure, you’ve lost some skills because of the illness you have, but you still have lots of skills left and you work with the skills you have.”
The-CNN-Wire
™ & © 2023 Cable News Network, Inc., a Warner Bros. Discovery Company. All rights reserved.