The RSV surge didn’t come out of nowhere, but gaps in data made it tougher to predict
The United States is dealing with a unique season of respiratory virus transmission: Flu cases are on the rise earlier than usual
By Deidre McPhillips and Jacqueline Howard, CNN
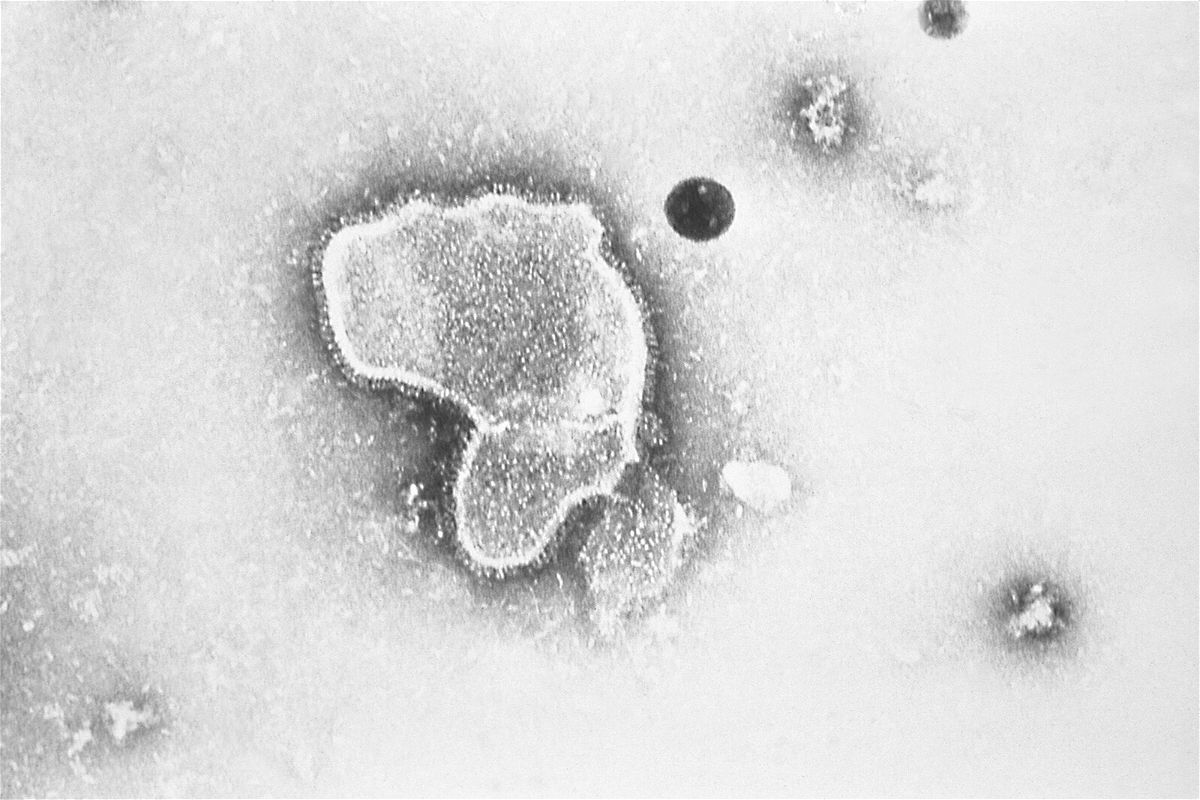
The United States is dealing with a unique season of respiratory virus transmission: Flu cases are on the rise earlier than usual, and RSV case rates are extra high, even after an “unprecedented” early surge this summer. And Covid-19 is still a public health emergency.
Public health experts expected a break from typical seasonal trends amid a pandemic that has disrupted “normal” in so many ways. Some outcomes were bound to be unpredictable.
But one thing that could help public health officials better prepare for and respond to these unusual surges is more complete and real-time disease surveillance that more acutely tracks trends in transmission and other key data points. It’s especially critical now, as the country faces what’s expected to be an especially rough winter when virus trends have shifted.
“The system has detected the changes appropriately, but the change itself is more unexpected,” said Janet Hamilton, executive director of the Council of State and Territorial Epidemiologists.
The Covid-19 pandemic revealed how fractured and undervalued the United States’ health data infrastructure is, and data lags made it difficult to respond swiftly to the coronavirus. Ultimately, the frequency of Covid-19 reporting — daily, sometimes hourly updates — created a flood of information that was shared throughout most of the pandemic.
But that was unique.
Surveillance systems for viruses like influenza and RSV were established long before Covid to track trends, with data that’s generally updated weekly. The national data is based on voluntary reporting from a few dozen labs that represent about a tenth of the the population, which is then shared by the US Centers for Disease Control and Prevention.
In typical years, this system captures what it’s meant to.
“In many ways, it works very well, because you can often determine a lot from a sampling strategy,” Hamilton said, especially with diseases that have been consistent over the years.
“For things like influenza and RSV, you don’t necessarily have to know about every person. But it is important to know are you starting to see circulation, is it increasing, how long are we seeing circulation for, is it peaking, and when is it going down.”
In atypical years like this one, more real-time information is critical — but the earliest signs of major outbreaks weren’t shared through surveillance data.
Matching form and function
Pediatric hospitals are among the most broadly affected by this unusual virus season.
About three-quarters of pediatric hospital beds are in use across the country, well above the average over the past few years. They’re more than 90% full in Rhode Island, Minnesota, Maine and Texas, as well as in Washington, DC, according to data from the US Department of Health and Human Services.
Hospitals are constantly evaluating capacity needs, preparing for infectious disease surges by making sure there are enough beds available and supplies in place to help those in need. But when it comes to planning ahead, experts say that getting more laboratories to participate in the national surveillance system isn’t the most critical need for hospitals.
“For hospitals [using CDC data], it’s a little like looking through the rearview mirror. They’ve already begun to experience that uptick in cases themselves before it’s noticeable in the federal data,” said Nancy Foster, vice president for quality and patient safety with the American Hospital Association.
“We’re talking about data that are collected inside hospitals, transmitted through a data trail to get to the federal government, analyzed there and then fed back to hospitals.”
Instead, hospitals rely on informal networks of physicians, public health leaders and others to share more immediate information about recent experiences to help make planning decisions.
There are efforts underway to identify and build upon critical lessons learned from the Covid-19 pandemic to help make key data available more immediately and reaction times more efficient, Foster said.
“Within those conversations, there have been discussions of how to take advantage of some of these clinican-to-clinican conversations and what you’re seeing on social media in order to identify potential surges or other related problems like supply shortages in more real-time so that they can be addressed more promptly,” she said.
In addition to managing the national surveillance systems, CDC and HHS are working with local partners to assess the impact of increased RSV infections, identify potential needs and provide resource support.
The CDC launched its Center for Forecasting and Outbreak Analytics in April, with an aim to be like the “National Weather Service for infectious diseases.” The group hasn’t yet worked with RSV data — it’s focused on Covid-19, monkeypox and Ebola for now — but said it can offer consultation as needed.
“As we continue to build our analytics infrastructure and workforce, CFA’s initial focus is on supporting the public health response to pandemic-prone diseases and outbreaks,” said Dylan George, the center’s director of operations.
Scientists use sewage to track RSV surges
One way to supplement traditional surveillance methods became more popular throughout the pandemic: tracking levels of virus shed in local sewage systems.
Weeks before the surge of RSV infections began sweeping the United States, researchers at WastewaterSCAN, a national wastewater monitoring initiative based at Stanford University, noticed a significant uptick in detections of the virus within wastewater across the country.
“We saw the beginning of RSV starting to tick up around the middle of August of this year,” said Marlene Wolfe, an assistant professor of environmental health at Emory University and co-principal investigator for WastewaterSCAN. “If we’re seeing it in wastewater, the infections are there. We just had data before clinical positivity data was reported.”
Wastewater surveillance can help hospitals with capacity planning, as they can track community wastewater data to determine when there could be an increase in the circulation of a certain infectious disease and prepare for a corresponding rise in sick people, Wolfe said. “One of the really important ways that we see wastewater data being used is for capacity planning. There are a lot of public health responses that you could take in response to knowing that there is an uptick in a disease.”
Also, because most people do not get tested for RSV — especially adults, for whom symptoms mimic a common cold — wastewater surveillance can help track when and where the virus is circulating.
Wastewater surveillance involves testing sewage to determine whether feces and other types of human waste in untreated sewage contain genetic material from viruses or bacteria that can make people sick. That material, either RNA or DNA, can be detected in the waste — but it does not indicate whether the pathogen is infectious in the water itself.
The WastewaterSCAN initiative, which contributes results to the CDC’s separate wastewater surveillance system, launched in November 2020 to scan sewage samples for SARS-CoV-2, the virus that causes Covid-19. Since then, the program has expanded to monitor dozens of sewage plants across the country and track more pathogens — including RSV testing in about 70 city and county sewage systems across 20 states.
“You can track RSV with wastewater. We have an abundance of evidence now that we’ve been able to do that very effectively for about a year, and it’s providing us right now in this season, in this outbreak, good information that aligns with our other sources of information about RSV and gives us a little bit of a jump on making sure that we have good information to prepare our communities,” Wolfe said.
“And the patterns that we’re seeing in where transmission is particularly high across the country from clinical reporting matches what we see across the country for locations where those levels are particularly high in wastewater,” she said. “So we are going to continue to build and expand the system to be able to give us that network of sites across the country that tell us where are the hot spots for these different diseases, whether it is RSV, influenza or Covid.”
Public health is local first
In any case, experts say that local data is the key to public health success.
“I always want to have more granular data and information — in particular because we are coming out of Covid and we’ve had such unusual respiratory disease seasons that having more granular data available would be helpful for determining exactly where we’re seeing differences,” Hamilton said.
“People respond more to local data. If people really feel like it’s next to them and with them, they’re often more willing to make behavior changes that you just don’t see if the danger doesn’t feel present.”
The states and jurisdictions that do have more robust surveillance systems in place noticed something unusual in their local trends in earlier years and “cobbled together funding” because they knew they needed to do more to understand it, she said.
But now, the trends have become unusual in most places, and robust systems aren’t in place to best understand them.
Changing that requires funding.
“We can do more and would like to do more,” Hamilton said, but “it’s scary, really, how under-resourced RSV surveillance is.”
The-CNN-Wire
™ & © 2022 Cable News Network, Inc., a Warner Bros. Discovery Company. All rights reserved.