Dr. Sanjay Gupta: While monkeypox cases rise, why are we waiting for the cavalry to rescue us?
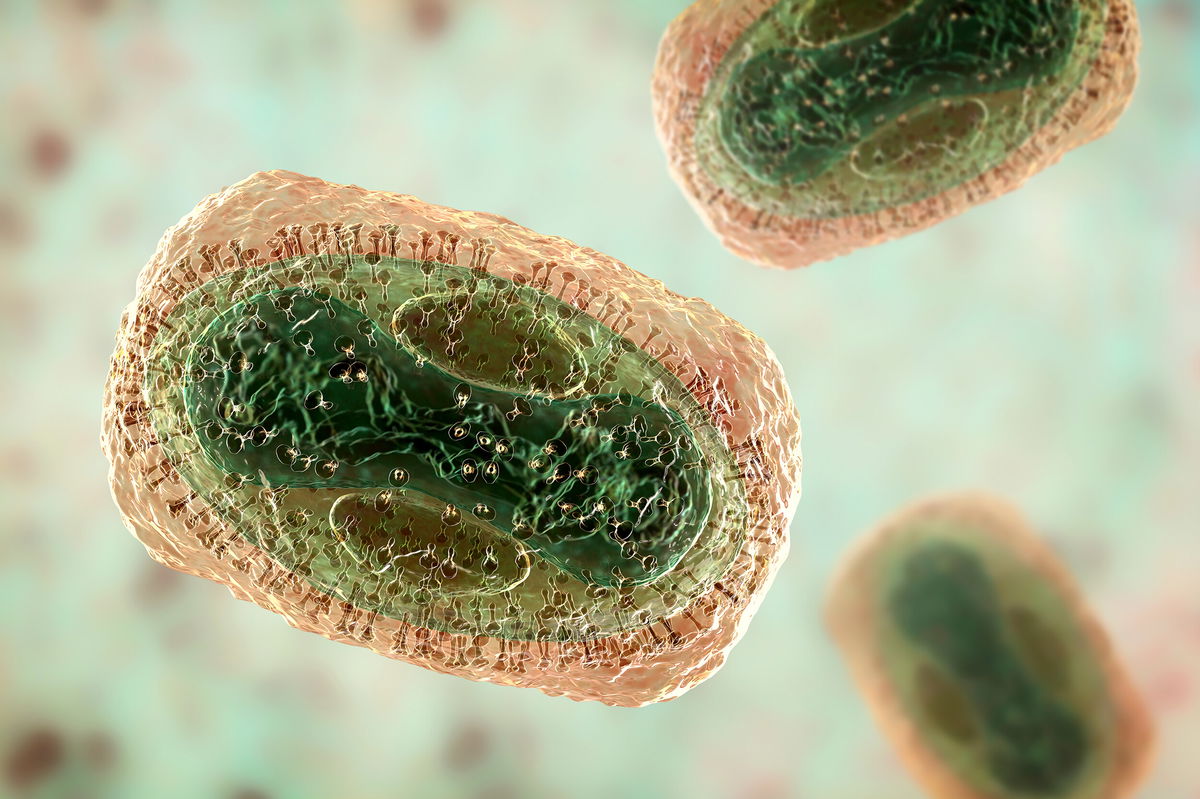
Monkeypox virus particles
By Dr. Sanjay Gupta, CNN Chief Medical Correspondent
It’s hard to believe we are face-to-face with a new health crisis, monkeypox, before we are even out of the woods with the previous — but still very much current — crisis, Covid-19.
The pandemic, which has held the United States and almost every other country in its grip, should have taught us valuable lessons about how to manage a public health emergency, but it seems we are making some of the same mistakes we made not even three years ago, when the SARS-CoV-2 virus started to spread.
Testing for the monkeypox virus, once very limited, is now more available, but underused. The demand for vaccines is outpacing the supply. There are nearly 2 million courses the highly effective TPOXX antiviral sitting in the Strategic National Stockpile, but many health care providers are still having a hard time getting the medication for their patients.
We are one of the wealthiest countries in the world, spending more than $4 trillion dollars a year on health care, more per person than anywhere else. With all those resources and technology, it’s not as if the United States is incapable of mounting a significant response to an emerging outbreak. And there is little doubt we will eventually do what should have already been done: declare monkeypox a public health emergency, appoint a national coordinator and mount a more significant response. But why do we wait so long, drag our feet and endure so much suffering in the meantime?
As I have learned over the past few years, there is a significant difference between preparedness and response, even though the two are often conflated. The United States is extraordinarily prepared, ranked No. 1 for pandemic preparedness in the 2021 Global Health Security Index.
Instead, we are leading in a different way. As of today, we have the most confirmed cases of monkeypox on the planet, more than 5,000. That is almost 25% of the global numbers, even though we are just under 5% of the world’s population.
It is now clear: Preparedness alone does not guarantee a rapid response. With Covid-19, and now monkeypox, we were too slow to respond. It was as if we are sitting in a turbo-charged Ferrari, capable of massive acceleration, but instead only idling in the driveway.
Cavalry culture
Over the past three years, we have witnessed something counterintuitive. It was predominantly wealthy countries that were hit hardest during the Covid-19 pandemic. They had some of the highest death rates, despite their enormous resources.
While there are many reasons for this, including misinformation, lack of public trust, and the entangling of public health and politics, I think there is something else, as well: We have adopted what I call a “cavalry culture.” We wait for the cavalry to ride in and rescue us, instead of taking smaller preventive steps — such as establishing modern and reliable data systems, mastering our supply chain along the way, and acting early to head off the outbreak in the first place.
If that sounds familiar, it’s because we too often do the same with our personal health matters. According to research published in The Lancet Public Health, nearly half of chronic disease in the United States is mostly preventable, with lifestyle changes. Even knowing that, however, the medical system is set up for the cavalry to come in with expensive medications and high-tech interventions, instead of providing equitable access and incentives for preventative care.
There are a couple of important axioms in public health. One is, by the time you think you must act to contain an outbreak, it is already too late. And, if you think you are overreacting, you are probably reacting just the right amount. In the case of Covid, and now monkeypox, we seem to have forgotten those basic public health principles. And, the real question now seems to be: When will the government finally hit the gas pedal on our highly tuned Ferrari?
I don’t want to suggest any of this is easy. There are significant issues of uncertainty and unpredictability. Much like a hurricane forming at sea, we often don’t know exactly where or how hard it will hit. We want to be measured, calm in our response and to cause as little disruption as possible. We want to be thoughtful and gather as much information as is available.
And therein lies one of our biggest problems: basic data. I have often wondered, how is it that a numbers-driven, high-tech country like the United States can’t get basic data right?
Data disaster
As long as I’ve been reporting on the Covid pandemic, I have always had to offer the caveat that case numbers are probably off, sometimes wildly so. We have probably never had a clear vision on just how widely the virus was spreading at any given time in the United States, and going into the fall 2022, the situation isn’t really any better.
In early July, the Institute for Health Metrics, a research center at the University of Washington, released a model suggesting that actual Covid-19 cases are seven times higher than reported cases. At times, it seems the tech platforms for Snapchat and Twitter offer more data analytics than the patchwork of state and federal systems that underpin the public health of our country.
“First, there’s a lack of data access needed to understand where disease outbreaks are spreading. This is due to data collection limitations that Congress needs to fix,” said Dr. Tom Frieden, president and CEO of Resolve to Save Lives and a former director of the US Centers for Disease Control and Prevention.
He said there is also a need to update analog systems and connect them to each other — getting them to speak the same language. Right now, it’s the Tower of Babel.
“Second, we lack sufficient numbers and, in some cases, skills of people and systems at the federal, state and local levels that can deliver services and communicate effectively with communities. Finally, we are in perpetual panic and neglect funding cycles,” he said.
As a result of all of the things Frieden is describing, our current data collection and reporting system leaves important information fractured into dozens of states and territories, and thousands of county pieces for the CDC to puzzle together.
“I have been struck as we at CDC are now conquering another public health challenge — monkeypox — as to how little authority we at CDC have to receive the data,” CDC Director Dr. Rochelle Walensky told the Washington Post.
Walensky is talking about basic data, like where the vaccine has gone, who has been vaccinated, whether the vaccine is working, and even monkeypox case data like who is getting infected, their age and race/ethnicity. Why might this be so?
“States don’t routinely share vaccine doses administered data with the federal government — Covid was really the first time that we were able to successfully put data use agreements in place,” Claire Hannan, the executive director of the Association of Immunization Managers, told CNN. Part of the reason is because “states have laws in place to protect identifiable information.”
Some information has been getting to the CDC, but it is challenging to get and incomplete. The CDC director told the Washington Post, “We have been speaking to our state and local partners probably at least three times a week, all of them. … That is not how you synthesize data. We need … standardization of those data, and we need to have those data come to us in a standardized fashion so that they can be connected, we can compile them and rapidly report them out. We cannot at CDC collect the data and make informed decisions by calling 64 jurisdictions, and honestly, 3,000 counties.”
The CDC is currently working on agreements that would broaden the agency’s access to states’ data, as they successfully did with Covid. Hannan explained, “The need to quickly get the [monkeypox] vaccine out left no time to get data sharing agreements in place.”
But even if those agreements were in place, it still doesn’t mean the states’ ability to actually obtain vaccine doses would be made any easier. That’s because the states wouldn’t be using the same data system for ordering and tracking doses they generally use. Because the US Department of Health and Human Services and the Administration for Strategic Preparedness and Response are in charge of monkeypox vaccine distribution, there would be yet another data system involved.
“They were asking states to request the vaccine using paper forms and email,” said Hannan. “They were asking states to complete forms [with fillable fields] on those who were receiving the vaccine and return these forms to the federal government.”
The problem was there weren’t even the right fields for the specific questions being asked, such as reason for vaccination or type of exposure or risk, Hannan said. It wasn’t that the necessary forms weren’t being filled out, it was that they couldn’t be filled out because of disparate data platforms.
It is a baffling level of bureaucracy in the middle of an unfolding outbreak.
Testing, vaccines, therapeutics
As things stand now, the issues with data collection, testing, vaccines, treatments and communication are sounding a lot like the ones we experienced with Covid-19.
But, to be clear, monkeypox is not that much like Covid. For now, it seems to spread primarily through sores or lesions during close, personal touch and shared objects like towels and linens, as well as respiratory secretions during prolonged face-to-face contact.
The monkeypox outbreak is also different for another fundamental reason. Unlike with Covid, which was caused by a novel virus, the basic tools already exist either for monkeypox or its close relative, smallpox. We didn’t have to build them from scratch. That means we could have had them or put them to better use by now.
Take testing. At the start of the outbreak, testing capability was capped at about 6,000 tests per week, which meant that doctors really had to ration them to a narrow group of people — primarily a subset of men who have sex with men. Since then, the CDC has partnered with five labs to scale up our capabilities and we should soon be able to process up to 80,000 tests a week. But the tests are being underutilized, according to CNN reporting. Experts blamed the low uptake on several factors, including a lack of awareness among doctors about the virus and the fear of stigma among patients.
So, just as with Covid, the real scope of the monkeypox outbreak is probably underappreciated. Confirmed or probable cases stand around 5,000, according to CDC data, but the number could be several fold higher.
Another tool that could be tremendously helpful is testing of wastewater. As we have seen with Covid, it can better define the scope of the outbreak and where it will emerge next. Two months into the outbreak, we still aren’t doing this widely for monkeypox.
And then there are vaccines. Unlike Covid, where we spent upward of $20 billion to develop, test and distribute vaccines, we already have a vaccine specifically approved for monkeypox.
Supplies were limited and the initial US vaccination strategy focused on known monkeypox cases and their immediate contacts. But the outbreak continued to grow, and the strategy had to change. The count of people eligible for the two-dose Jynneos vaccine has now expanded to an estimated 1.5 million.
With that same cavalry culture, we are woefully behind in getting those doses to people who want them. At this time, only 336,710 doses have been shipped to states. Ordering only just began for about 800,000 more doses. This scarcity has created long lines in monkeypox hotspots like New York City, which has the highest number of cases in the country.
It also means that the vaccine, which can be given within 14 days of exposure (but preferably within four) to prevent or reduce the severity of disease, is currently being used more as a treatment — a post-exposure prophylaxis — rather than as a real preventive measure.
As National Institute of Allergy and Infectious Diseases Director Dr. Anthony Fauci said on CNN, that focus will have to shift.
“It’s very clear with the spread of this that there now has to be a balance between vaccines available for those who clearly have been exposed, as well as those at risk,” Fauci said. “What you want to do is a balance between vaccinating those who clearly have had an exposure but go well beyond that.”
It’s a missed opportunity that won’t be rectified immediately, even with the soon-to-arrive 786,000 doses announced by HHS this week. Needs will still outstrip supply.
Finally, there is the issue of treatment. The CDC has made the antiviral smallpox treatment tecovirimat, called TPOXX, available to monkeypox patients who have or are at high risk of severe disease under an “alternate regulatory mechanism.”
There are 1.7 million courses of TPOXX stockpiled. But once again, getting the medication to patients who could immediately benefit has proven to be bureaucratically burdensome for both patients and providers.
“You’re talking about a five, six-day time lag to get that medication to you at a local doctor’s office, no matter where you are. And the paperwork, and all of the bureaucracy to make that happen is very cumbersome, takes a few hours of your time. And that’s the barrier,” Dr. Stacy Lane, founder of the LGBTQ-centered Central Outreach Wellness Center in Pittsburgh, told me recently.
Fortunately, those rules were loosened somewhat last week, allowing patients to get treated more quickly and reducing the amount of documentation needed. The CDC and the US Food and Drug Administration are working to further streamline the process.
In the meantime, though, patients are suffering. Even though most cases are “mild,” they are still uncomfortable, or downright painful, depending on where sores appear. Plus, there is a risk of long-term complications if the pox lesions develop in areas around the eye or GI tract.
All of these gaps have the hardest hit community on edge.
“Largely public health officials know how this has spread. They know how to vaccinate people … we know how to treat it, and we know how to prevent it,” says Samuel Garrett-Pate, managing director of external affairs of Equality California, the largest statewide LBGTQ+ civil rights organization.
“It unfortunately seems that despite two years of building up our public health infrastructure to prevent what happened with Covid-19 from ever happening again, despite the fact that we are better prepared in terms of already having a vaccine available, the CDC and FDA seem to be caught flat-footed once again. And I think as a result, you’re seeing very real and understandable fear anxiety among the LGBTQ community.”
Is it too late?
Dr. Scott Gottlieb, a former FDA commissioner and current board member of Pfizer, has been pessimistic about the trajectory of monkeypox in the United States.
“We’re now at the cusp of this becoming an endemic virus, where this now becomes something that’s persistent that we need to continue to deal with. I think the window for getting control of this and containing it probably has closed and if it hasn’t closed, it’s certainly starting to close,” he said on Face the Nation on July 17.
CDC’s Walensky pushed back on Gottlieb’s assessment calling it “misinformed and off base,” saying that while it’s true there is much work to do, the US has made dramatic progress on priorities like testing, vaccines and education.
There has been measurable progress in these areas, no doubt. But, I do worry that we once again waited too long. We sat idling in our Ferrari, perhaps not wanting to believe that somehow we had suddenly found ourselves in the middle of yet another outbreak.
I remember when I first saw a case of monkeypox — it was in 2008, in the Democratic Republic of the Congo, one of the handful of countries in Africa where the disease is endemic. To tell you the truth, I never thought I would see it in the United States. After all, it was a virus that hadn’t traveled much since it was first identified in DRC in 1970. My guess was that most of my medical colleagues in the United States would likely only see pictures of the distinctive pox lesions in textbooks.
The world, however, is changing, as we have been reminded of twice in the last few years. There are new pathogens emerging, and existing pathogens are more easily traveling the world.
We have learned painful lessons in the last few years, and we are now in the midst of our first significant test since the Covid pandemic began, to see if we do any better this time around.
There is no doubt we are capable, and we are prepared. The question is will we use all those remarkable resources and respond, or we will wait and suffer until the cavalry has to rescue us once again?
The-CNN-Wire
™ & © 2022 Cable News Network, Inc., a WarnerMedia Company. All rights reserved.
CNN Health’s Andrea Kane contributed to this report.

